

GLASGOW COLORECTAL CENTRE
Scotland’s Best Private Colorectal Surgery & Colonoscopy Clinic
info@colorectalcentre.co.uk
If you have any questions, call Catherine on 0735 506 6597

© Glasgow Colorectal Centre. All Rights Reserved

 Book an Appointment
Book an Appointment
Any questions? Call Catherine on 0735 506 6597
Info@colorectalcentre.co.uk
What is an anal fissure?
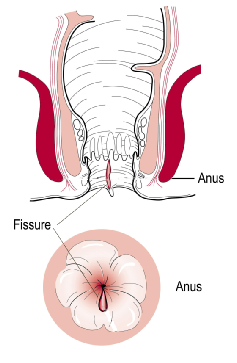
An anal fissure is a crack, tear or cut in the lining of the anus (back passage). A fissure may be acute or chronic, depending on how long it has been present. Sometimes, the skin at the bottom of the fissure may become swollen which may give the mistaken impression that the pain and bleeding are due to piles or haemorrhoids.
Why do anal fissures occur?
Fissures can occur at any age, but most commonly occur in young children and adults. Many fissures occur for no particular reason. However, direct trauma to the area may be a factor in many cases. Anything that can cut or irritate the inner lining of the anus can cause a fissure. Most commonly constipation leading to a hard, dry bowel movement may cause a fissure. 
Other causes of a fissure include diarrhoea or inflammatory conditions of the anal area. Fissures may also develop after delivery of a baby (post partum). Anal fissures may be acute (recent onset) or chronic (present for a long time or recurring frequently). Chronic fissures often have a small external lump associated with the tear called a sentinel pile or skin tag. This is commonly mistaken for standard piles or haemorrhoids
What are the symptoms of an anal fissure?
The symptoms of a fissure are pain, especially when passing a bowel motion, and some bleeding. Occasionally, people experience discharge of an abscess in association with a fissure. Fissures are quite common, but are often confused with other causes of pain and bleeding, such as piles or haemorrhoids. Patients may try to avoid defecation because of the pain.
How is an anal fissure treated?
Often treating the constipation or diarrhoea can cure a fissure. An acute fissure is usually managed with dietary changes and local creams (non-
A number of specific creams have come on the market over the last few years. These have been designed to reduce the spasm within the anal sphincter and can heal up to 80% of fissures. Some fissures, if they do not respond to these methods, may require an operation. The most commonly used ointments are
- Rectogesic: (0.4 per cent GTN -
(glyceryl tri- nitrate)). This may cause headaches if not used according to instructions. An information sheet on using GTN ointment for anal fissure is available here. Additional information is available on NHS choices website - Anoheal (2% diltiazem cream). This is better tolerated although some patients develop skin irritation with the cream. An information sheet on using diltiazem cream for anal fissure is available here.
How successful is non-operative treatment for anal fissure?
Fissures can recur easily, and it is quite common for a healed fissure to recur after a hard bowel movement. Even after the pain and bleeding has disappeared one should continue to aim for good bowel habits and adhere to a high fibre diet or fibre supplement regimen. If the problem returns without an obvious cause, further assessment may be needed.
What can be done if a fissure doesn’t heal?
A fissure that fails to respond to treatment should be re-
What types of operation are performed for anal fissure?
An operation may be necessary in order to get a more detailed look at the fissure and possible take a biopsy. This is called an Examination under Anaesthesia (EUA). Your colorectal surgeon may also recommend additional measures including injection of the anal sphincter with Botox. This relaxes the anal sphincter muscle and may heal up to 85% of fissures. The effect is transient (8-
Persistent fissures may require a lateral internal anal sphincterotomy. This is a highly effective treatment for a fissure and recurrence rates after this type of surgery are low. Surgery usually consists of a small operation to cut a portion of the internal anal sphincter muscle (a lateral internal sphincterotomy). This is a fairly minor operation and most cases can be performed as a day case without the need to stay overnight. This sphincterotomy operation helps the fissure heal by decreasing pain and spasm which improves the blood supply to the skin.
A small percentage of patients who undergo a sphincterotomy may find impaired control of the bowel motions after operation (minor faecal incontinence). Surgery is not therefore usually performed without first trying non-
Other operations, less frequently performed, include anal stretch or anoplasty. If a sentinel pile is present, it too may be removed to promote healing of the fissure. This may be combined with either injection with Botox or sphincterotomy.
What are the complications of surgery for anal fissure?
A small number of patients who undergo injection of the anus with Botox may experience transient weakness in the sphincter muscle and some incontinence of stool.
As discussed above, sphincterotomy also infrequently may interfere with one’s ability to control bowel movements. Patients who have had previous anorectal surgery or women who have sustained a preceding injury to the anal sphincter during childbirth may be at increased risk of these problems.
Surgery is generally very safe. However, all surgical treatments do have other risks, and your colorectal specialist will address these with you.
How long does the healing process take after surgery for anal fissure?
Complete healing occurs in a few weeks, although pain often disappears after a few days
Can fissures lead to colon cancer?
No! Persistent symptoms, however, need careful evaluation since conditions other than fissure can cause similar symptoms. Your doctor may request additional testing even if your fissure has successfully healed. A colonoscopy may be required to exclude other causes of bleeding.
Can I be treated for anal fissure at the Glasgow Colorectal Centre?
Yes. Glasgow Colorectal Centre surgeons’ Richard Molloy and Graham MacKay are happy to assess patients with an anal fissure and will advise on investigation and management, be it medical treatment or surgery including injection of the fissure with Botox.

Anal Fissure
Causes, symptoms, diagnosis and treatment

If you have any questions about anal fissure or other colorectal issues, your own GP is often the best first port of call.
If appropriate, they will be able to arrange a referral to a colorectal specialist centre such as the Glasgow Colorectal Centre.
An anal fissure is a small tear, cut or crack in the skin that lines the anus (back passage). Although anal fissures may occur at any age, most commonly they occur in children and young adults. Anal fissures can give rise to severe pain and rectal bleeding or blood in stools when passing a bowel motion.
Treatment aims to avoid constipation by increasing fibre and using laxatives to soften the stool. Special creams such as Rectogesic (GTN ointment) and Anoheal (diltiazem) can relieve pain and spasm and can speed healing. Most fissures settle with medical treatment but occasionally, an operation may be necessary. Injection of the anus with Botox can help relieve spasm and induce healing. Occasionally, a sphincterotomy operation (small cut in the anal sphincter muscle) is required to heal a chronic fissure.
